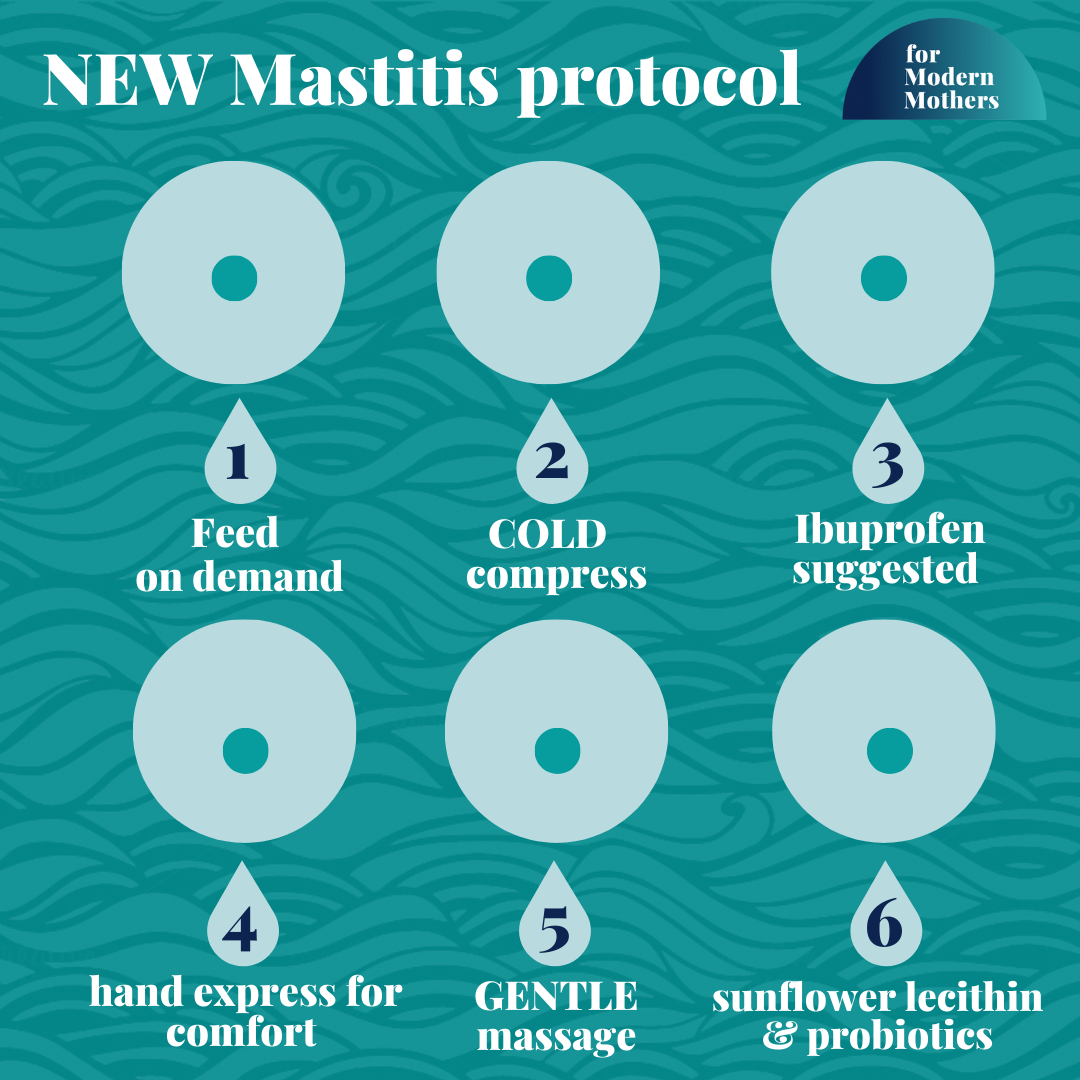
The NEW Mastitis protocol
As you probably already know, I always like to keep you up to date & informed. Making sure you have the latest information and guidance so you can make the right decisions for you and your baby. Because that’s super important.
This one is all about breastfeeding, and about a recent update to the Mastitis protocol. It’s important as it actually turns-on-it’s head a lot of the previous recommendations for Mastitis. Also because the NICE guidelines have not yet been updated, and also many GPs have not been updated either (who are the first port of call for folks with mastitis).
Why the changes?
These changes have been made to the clinical protocol for Mastitis by the ABM as there have been several key changes that significantly shift what we thought we knew about Mastitis. Because science and knowledge moves on doesn’t it. Mastitis is now described as a spectrum - not one sole thing. Oversupply (hyperlactation) is the first marker, this can then lead to painful inflammation which causes narrowing of the milk ducts (previously called a ‘plugged duct’), which could then progress to inflammatory mastitis.
So what we previously called ‘plugged ducts’ are now more accurately described as “ductal narrowing,” which means that using cold compress and other anti-inflammatory treatments should be used to manage mastitis instead of what was previously advised in guidance - heat (the opposite!). Also that we previously were advised that extra pumping was the way to go that would help to drain/unblock the breast - we know know that may actually exacerbate the problem. Similarly vigorous massaging is now thought to actually just be more uncomfortable and painful - and not actually help solve the problem!
So what is the new guidance then?
Feed on demand
As oversupply is now considered to be the first marker on mastitis spectrum we don’t want to do lots of extra pumping which could signal the body to continue to produce even more milk and perpetuate the cycle. Instead feed your baby on demand or pump on your normal schedule, and minimize extra pumping.
2. Use ice instead of heat for inflamed ducts & inflammatory mastitis
A hot/warm compress used to be the advice. But because heat doesn’t help reduce inflammation the recommendation when you have a painful plugged duct (which is actually a duct narrowing due to inflammation) is now to use COLD to tackle that swelling instead, which will reduce the blood flow and swelling. So you could use ice packs or a cold compress.
3. use ibruprofen
Plugged ducts are actually an inflammation (not a milk blockage as previously thought) so using NSAIDs such as ibuprofen can help.
4.Hand express
If you need to relieve discomfort from your breasts then doing this via hand expression is now advised, so you can be gentle and also not overstimulate.
5. gentle massage only
Be gentle with your massage! Those days of using the intensity of a shower head to massage your boobs, or grabbing an electric toothbrush to try to forcefully massage out your clogged duct are now gone. Infact those things can make the problem worse according to the updated guidelines.
“Attempts to extrude a ‘plug’ or milk precipitate by squeezing or aggressively massaging the breast are ineffective and result in tissue trauma,” note the new guidelines authors.
So instead the guidance now is to try gentle, lymphatic draining massage which involves “a light sweeping of the skin rather than deep tissue massage.” Sweep up from the nipple toward the armpit to help drain any extra fluid and calm the inflammation.
6. Sunflower Leicithins and probiotics
It used to be that antibiotic were advised immediately for mastitis, and sometimes as a precautionary measure. But the new protocol says that actually antibiotics may not always be required (only reserved for what’s called ‘bacterial mastitis’ - see more below on this type of Mastitis) and not for inflammatory mastitis nor for mastitis prevention.
It’s now said that you should consider taking probiotics for mastitis prevention (and I suggest looking into probiotics to so many mothers in my mum & baby classes already for other reasons too). “A systematic review suggested that probiotics may be effective for both treatment and prevention of mastitis, but a strong recommendation could not be made due to limitations of the studied trials.” Specific strains that have clinical research supporting their use with mastitis include: Limosilactobacillus fermentum (formerly classified as Lactobacillus fermentum) or, preferably, Ligilactobacillus salivarius (formerly classified as Lactobacillus salivarius) strains.
Sunflower Lecithin has been recommended to combat recurrent plugged ducts. The usual recommended dosage for recurrent plugged ducts is 3600-4800 mg lecithin per day, or 1 capsule (1200 milligram) 3-4 times per day. After a week or two with no blockage, you can reduce the dosage by one capsule. If there is no blockage within another 2 weeks you can reduce it again by one. You may need to continue taking 1-2 capsules per day if stopping the lecithin leads to additional plugged ducts (info on dosage from KellyMom).
Lecithin is a very common food additive, and is found naturally in many other foods. There are no known contraindications to its use by breastfeeding mothers.
The reason why lecithin may help resolve and prevent plugged ducts is not clear. The well respected Dr. Jack Newman, says “It may do this by decreasing the viscosity (stickiness) of the milk by increasing the percentage of polyunsaturated fatty acids in the milk.” Lecithin is an emulsifier (used to keep fats/oils dispersed and in suspension): phospholipid molecules (such as lecithin) contain hydrophobic and hydrophilic elements; the hydrophobic portion has an affinity for fats and oils, and the hydrophilic portion has an affinity for water.
You can read more about Sunflower Lecithin here: https://kellymom.com/nutrition/vitamins/lecithin/
Antibiotics may not always be necessary
According to the new guidance “Use of antibiotics for inflammatory mastitis disrupts the breast microbiome and increases the risk of progression to bacterial mastitis.” Antibiotics also shouldn’t be used for mastitis prevention. Many antibiotics also boast anti-inflammatory properties, “and this may explain why women experience relief when taking these,” state the protocol authors.
THE Signs of bacterial mastitis
You may be experiencing a bacterial mastitis infection if you notice the following symptoms:
Abnormal swelling and/or a wedge of redness on the breast
A painful lump on the breast or general breast tenderness
Pain or burning while breastfeeding
A breast that feels unusually warm or hot to the touch
General malaise or flu-like symptoms
Chills
Fatigue
Fever
Bacterial mastitis may require antibiotics. So if you have any of these symptoms please contact your GP quickly to check and for treatment recommendations - which may include antibiotics.
You can take a look at the new mastitis protocol here yourself for more details:
https://www.bfmed.org/assets/ABM%20Protocol%20%2336.pdf
In a nutshell breastfeeding should not be painful. So if you do have pain, or think you may have symptoms of an infection contact a lactation professional or your GP for a consultation. You don’t have to do this on your own - help is there for you, please remember that. It’s probably the most important thing I tell people on my Empowered Breastfeeding Workshop that’s part of my Hypnobirthing & Antenatal Course
Most folks need some help and support at some point in their breastfeeding journey. You can find a lactation consultant here if you need one- https://lcgb.org/
If you need any other sign posting to support, please just let me know.
Susan x